Cognitive Behavioral Therapy (CBT) in Recovery
Recovery from substance abuse or mental health challenges often hinges on addressing both the mind and behavior holistically. Cognitive Behavioral Therapy (CBT), with its evidence-based techniques, serves as a cornerstone in this endeavor.
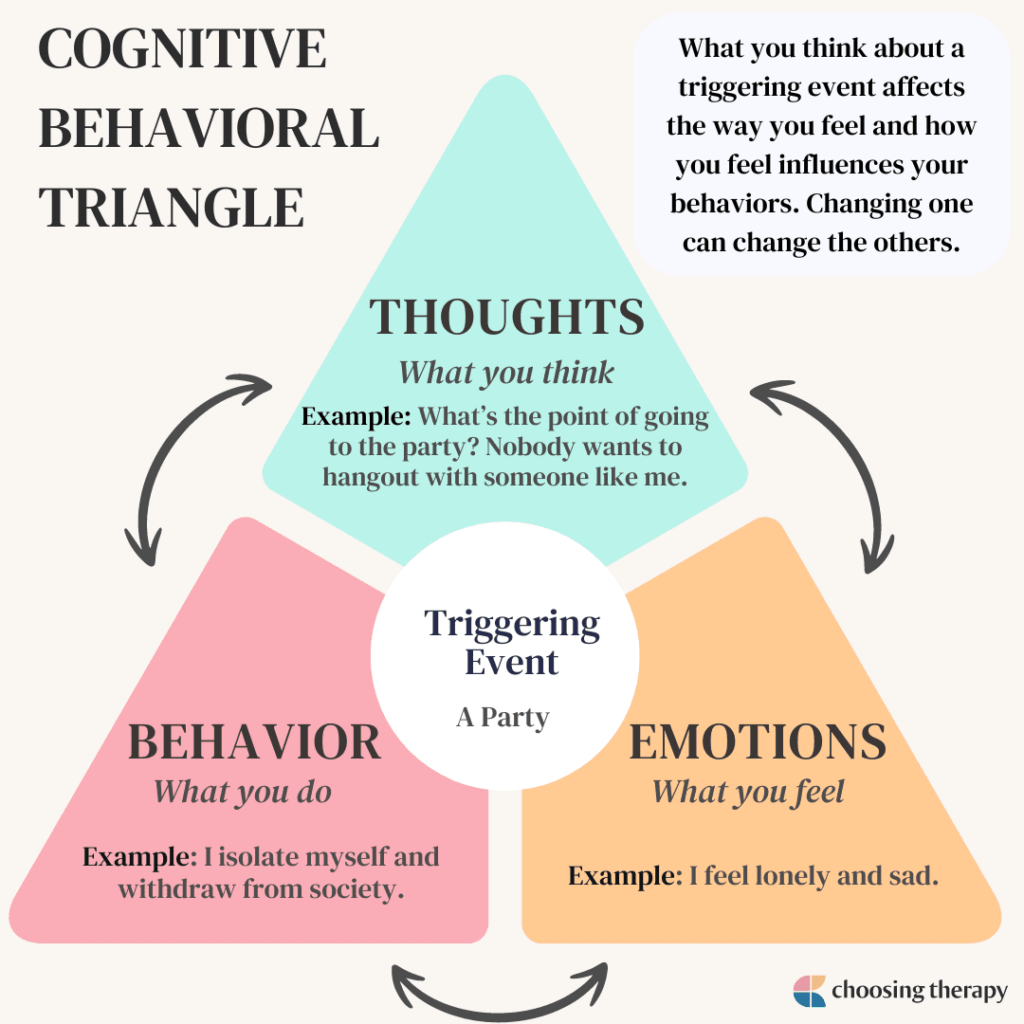
CBT is a structured therapeutic approach that focuses on helping individuals identify, challenge, and change detrimental thought patterns and behaviors. Rooted in the understanding that our thoughts, feelings, and actions are deeply interconnected, CBT aims to foster positive changes by addressing the negative patterns that perpetuate them.
Understanding Cognitive Behavioral Therapy (CBT)
CBT has proven effective in managing problems like depression, anxiety, and substance misuse. By developing new, healthier ways of thinking and behaving, individuals can significantly decrease the intensity of negative emotions and cultivate a life of acceptance, resilience, and change.
Key Components of CBT:
- It’s evidence-based, with extensive research supporting its effectiveness.
- It’s usually short-term, focusing on specific issues.
- It provides individuals with tools and strategies to navigate challenges.
- It empowers individuals to be active participants in their recovery.
Principles of CBT:
- Behavioral Activation – Engage in activities that counteract negative thoughts and feelings.
- Reflect: What activities lift your mood or perspective?
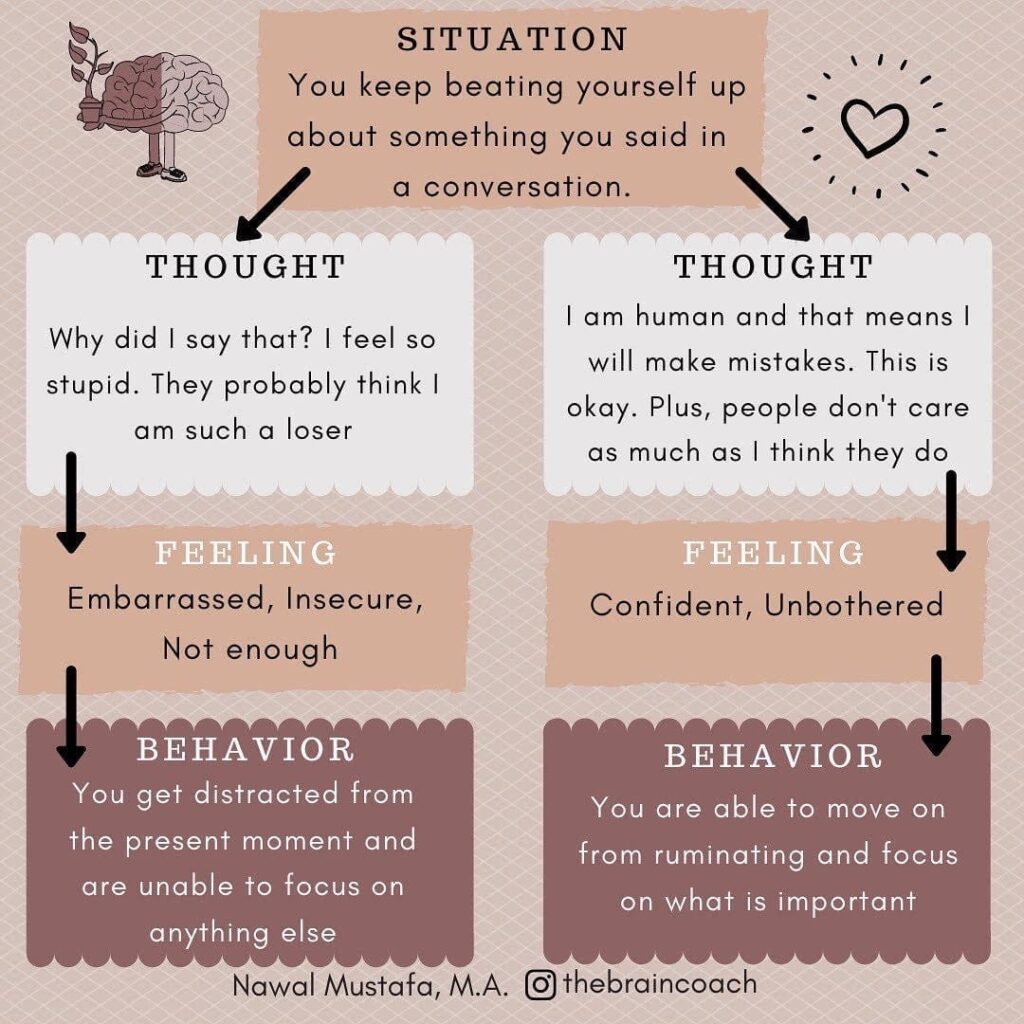
- Cognitive Restructuring – Challenge and replace unhelpful thoughts with more balanced ones.
- Reflect: How can you reframe a negative thought you had today?
- Problem-solving – Actively address challenges rather than avoiding them.
- Reflect: Is there a challenge you’ve been avoiding?
- Relaxation Techniques – Learn to manage and reduce anxiety and stress.
- Reflect: How do you currently cope with stress?
- Exposure Therapy – Face and reduce fears or avoidance of certain situations.
- Reflect: What fear can you address step-by-step?
- Skills Training – Equip yourself with tools for communication, assertiveness, and more.
- Reflect: Which skill would most benefit your current situation?
The Serenity Prayer and CBT The principles of CBT resonate with the sentiments of the Serenity Prayer, emphasizing acceptance, courage, and wisdom in the face of life’s challenges.
Serenity Prayer
“God, grant me the serenity to accept the things I cannot change,
Courage to change the things I can, And wisdom to know the difference.
Living one day at a time, Enjoying one moment at a time,
Accepting hardship as a pathway to peace,
Taking, as Jesus did, This sinful world as it is, Not as I would have it,
Trusting that You will make all things right, If I surrender to Your will,
So that I may be reasonably happy in this life,
And supremely happy with You forever in the next. Amen.”
The Role of Cognitive Behavioral Dialect Therapy (CBDT)
CBDT, an offshoot of CBT, integrates aspects of dialectical behavior therapy. It emphasizes balancing acceptance and change, especially beneficial for individuals with complex, co-occurring disorders.
Principles of CBDT:
- Cognitive Awareness – Recognize and identify negative thought patterns.
- Reflect: Can you spot a recurring negative thought in your day?
- Behavioral Activation – Engage in activities that counteract negative thoughts and feelings.
- Reflect: What activities lift your mood or perspective?
- Cognitive Restructuring – Challenge and replace unhelpful thoughts with more balanced ones. R
- Reflect: How can you reframe a negative thought you had today?
- Problem-solving – Actively address challenges rather than avoiding them.
- Reflect: Is there a challenge you’ve been avoiding?
- Relaxation Techniques – Learn to manage and reduce anxiety and stress.
- Reflect: How do you currently cope with stress?
- Exposure Therapy – Face and reduce fears or avoidance of certain situations.
- Reflect: What fear can you address step-by-step?
- Skills Training – Equip yourself with tools for communication, assertiveness, and more.
- Reflect: Which skill would most benefit your current situation?
More about CBDT:
- Origin: CBDT, which stands for Contextual Behavior Dialectical Therapy, is a therapeutic approach that combines elements of Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT).
- Balancing Act: Central to CBDT is the balance between acceptance of current feelings and situations (as in DBT) and the drive for change (as emphasized in CBT).
- Co-occurring Disorders: CBDT is particularly beneficial for individuals who face complex, co-occurring disorders. This might include, for instance, individuals with substance abuse issues alongside mood or personality disorders.
- Acceptance: Similar to DBT, CBDT emphasizes radical acceptance – which means fully and completely accepting reality as it is, even if it’s painful or difficult.
- Behavioral Focus: Drawing from CBT, CBDT focuses on identifying and changing negative thought patterns and behaviors. This provides patients with actionable steps to improve their mental health.
- Dialectics: A core principle borrowed from DBT, dialectics involves finding the middle ground between two opposites, recognizing that two seemingly contradictory things can be true at the same time.
- Skills Training: CBDT often incorporates skills training, similar to DBT, teaching patients practical skills in areas such as emotion regulation, interpersonal effectiveness, distress tolerance, and mindfulness.
- Holistic Approach: CBDT is a holistic therapy, addressing both the acceptance of negative thoughts and feelings, and the actionable steps a person can take to change problematic behaviors or thought patterns.
- Flexibility: The integration of multiple therapeutic approaches in CBDT allows for flexibility in treatment. Therapists can adjust the balance of techniques to best fit the needs of individual patients.
- Targeted Audience: While CBDT can be effective for a variety of mental health issues, it’s especially beneficial for individuals who might not have responded fully to traditional CBT or DBT alone.
Safety and Exploration in CBT For those engaging in CBT, feeling safe during the exploration of thoughts and behaviors is paramount. As with mindfulness, the importance of a supportive environment can’t be overstated. The therapeutic relationship in CBT is collaborative, where the therapist and client work together to identify and challenge unhelpful patterns.
Cognitive Behavioral Therapy (CBT) and mindfulness are both therapeutic approaches, but they differ in their origins, goals, and techniques. Here’s a breakdown of the main differences between the two:
CBT vs. Mindfulness: A Comparative Look
1. Origins:
- CBT:
- Born in the mid-20th century, CBT merges principles from behavioral therapy and cognitive therapy. Originally formulated to address depression, it later evolved to treat other conditions.
- Mindfulness
- With origins going back over 2,500 years to Buddhist traditions, its popularity in the West is relatively recent. It has now seamlessly integrated into Western psychotherapy.
2. Primary Focus:
- CBT:
- Concentrates on recognizing and rectifying negative thought and behavior patterns.
- Mindfulness:
- Encourages cultivating awareness of the present moment, be it positive or negative.
3. Techniques and Interventions:
- CBT:
- Employs strategies such as cognitive restructuring, behavioral activation, and exposure therapy.
- Mindfulness
- Leverages meditation practices, including body scans, breath-focused seated meditations, and walking meditation, urging the observation of one’s thoughts and feelings.
4. Goal Orientation:
- CBT:
- Solution-driven, it provides patients with tangible skills to tackle specific challenges, such as anxiety, depression, or phobias. It often has a predetermined number of sessions to reach therapeutic milestones.
- Mindfulness:
- Traditional mindfulness practices lack a specific “goal” in the way CBT does. Being in the moment is the primary objective, leading to benefits like reduced stress.
5. Integration
- CBT and mindfulness, although distinct, have found convergence. Mindfulness-Based Cognitive Therapy (MBCT) stands out, combining mindfulness techniques with CBT practices to combat the recurrence of depression.
Some points to ponder:
- Every challenge is an opportunity for growth.
- Thoughts are just thoughts; they don’t define you.
- You have the power to change unhelpful patterns.
- Your journey is unique, and every step is progress.
Safety and Boundaries in Recovery Navigating the recovery journey requires an understanding of personal boundaries. With CBT, individuals are empowered to recognize situations that may trigger negative thoughts or behaviors and to set healthy boundaries to protect their well-being.
Remember:
- Your boundaries are valid and essential.
- It’s okay to seek help when needed.
- Recovery is a journey, not a destination.
On this path of recovery, as you delve into the techniques of CBT or explore other therapeutic modalities, know that [Your Organization or Name] is here to support you, offering tools and resources to aid in your transformative journey.
Key Takeaways
CBT offers tangible techniques to address and modify harmful behavioral and cognitive patterns, while mindfulness promotes a non-judgmental awareness of the present. Both have their unique strengths, and together they offer a comprehensive approach to mental well-being.
As you embark on this transformative journey of recovery, whether you’re delving into the methodologies of CBT, embracing the serenity of mindfulness, or exploring their synergies, know that Precision P2P is here to guide and support you. We’re committed to providing you with tools, resources, and expertise every step of the way.
- For further research on Cognitive Behavioral Therapy (CBT), here are some resources:
- CBT Techniques and Tools